SHIFTING THE PARADIGM
IN HOW SURGEONS FINISH THEIR PROCEDURES
Explainer Video
Product Animation video
Demonstration
Presentation
Over 127 peer reviewed studies show significant benefits from abdominal wall blocks.
- 67% reduction in post-op opiate use vs local infiltration 5
- Over 70% of patients report being pain free at 1 hour after laparoscopic surgery 6
- Abdominal blocks tripled the time to first rescue analgesia 7
- Patients were discharged significantly earlier 8
- Rectus Sheath Blocks can provide sufficient pain control without the need for any other post-op analgesia 1
Why isn’t every surgeon doing an abdominal wall nerve block?
Ultrasound guidance is impractical. It requires extra equipment, adds extra costs and can delay surgery by over 18 minutes. 9
Blind Loss of Resistance techniques such as the “Pop-Pop” are inaccurate
and dangerous.
Local anesthesia is delivered to the correct plane only 14-24% of the time, and 18% of injections believed to be in the correct plane were actually intraperitoneal. 10
Pain free laparoscopy is possible with targeted nerve blocks 15
The thickness of abdominal wall fat and muscle at the umbilicus varies by over 50mm. 4 Current methods for targeting the posterior rectus sheath are inefficient and dangerous, because they approach the nerves from the anterior wall. The wide variation in fat and muscle thickness make blind injections highly inaccurate.
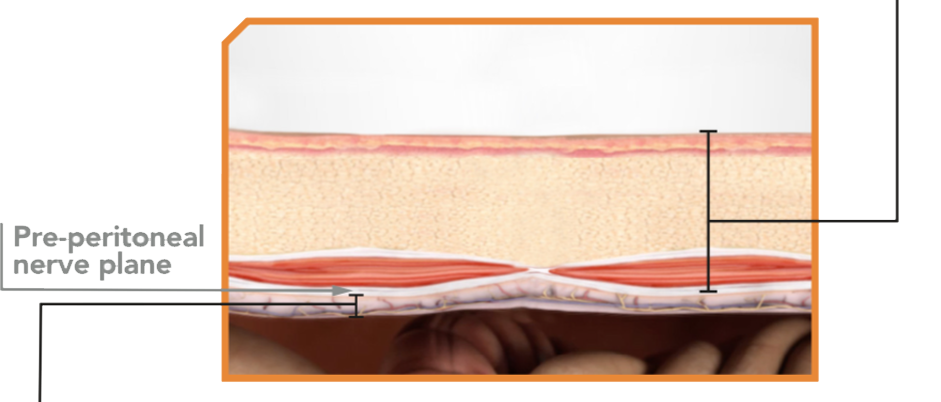
The distance from the peritoneum to the deep nerve plane varies by only 4mm. 3 When measured from below, the extreme variation due to fat and muscle thickness is eliminated and the nerve plane can be consistently targeted.
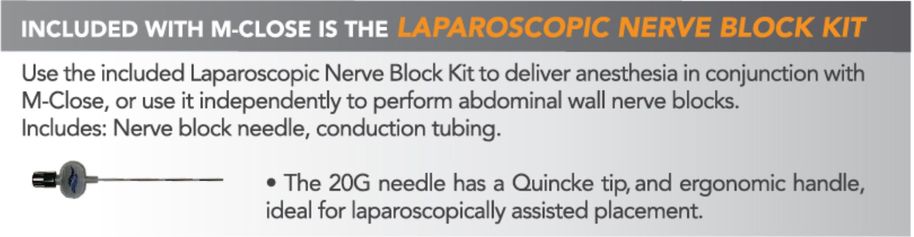
M-CLOSE uses a patented reference plane system, which positions the Nerve Block Needle relative to the peritoneum, not the skin surface.
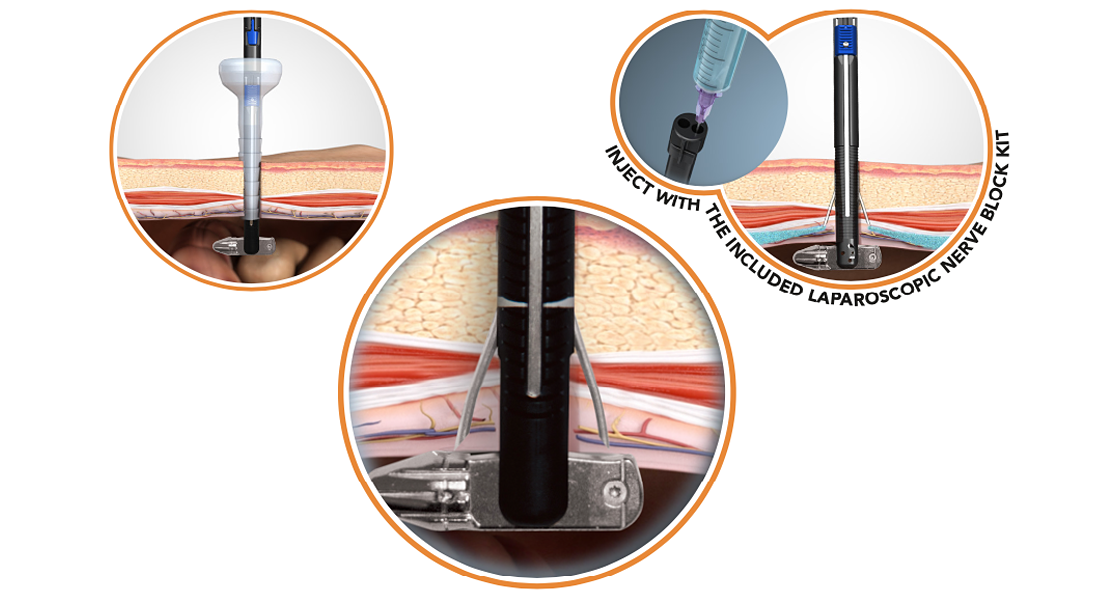
M-CLOSE KIT combines targeted anesthesia delivery with the most advanced port closure device 11
M-CLOSE PROVIDES A GOLD STANDARD CLOSURE 11
- Adheres to the Jonsson-Israelsson rules of fascial closure
- Suture bites are symmetrical and 1cm from each side of the defect
- Knot is above the fascial plane

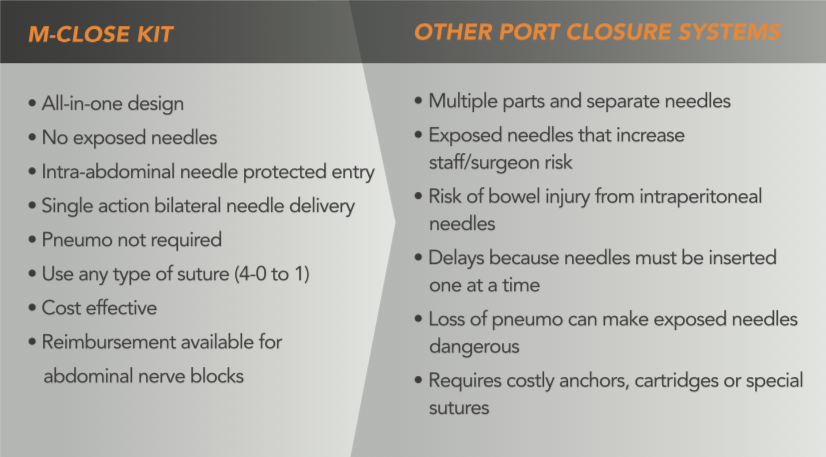
M-CLOSE IS SAFE
- No exposed needles help prevent sharps injuries
- Shielded needles can help prevent injury to intra-abdominal organs, even without pneumoperitoneum, or direct visualization 13
M-CLOSE IS EASY
- <30 seconds to place the suture
- Deploys two needles at once
- Can place multiple sutures for large defects
M-CLOSE KIT SAVES MONEY
- Costs less than most port closure devices
- Reduce costs related to post-op port site complications
- Save O.R. time by closing ports faster and avoiding unnecessary scope exchanges
- Deliver targeted anesthesia at no extra cost
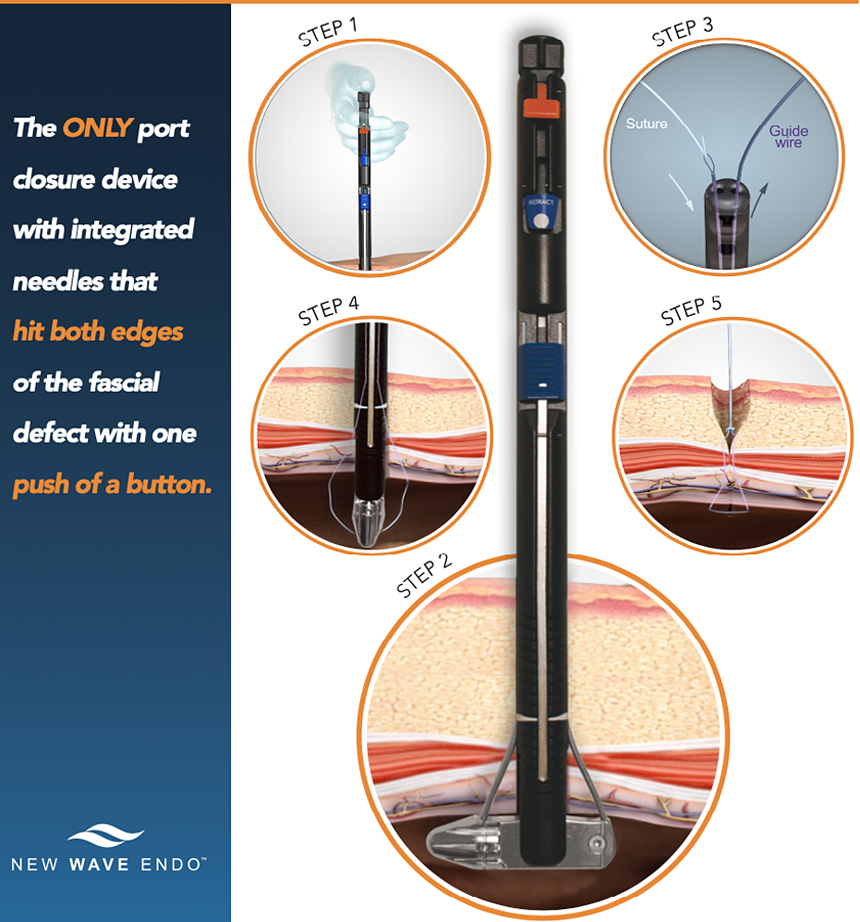
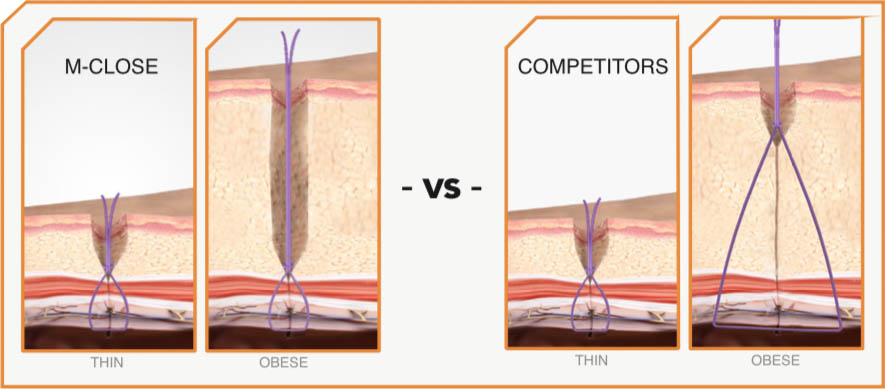
M-CLOSE KIT is designed for OBESE PATIENTS
Current devices use the skin as a reference, resulting in large suture bites as the abdominal wall gets thicker. These large suture bits increase pain and can loosen over time.
M-Close uses the fascia as a reference to produce suture loops that are always the SAME SIZE, regardless of abdominal wall thickness.
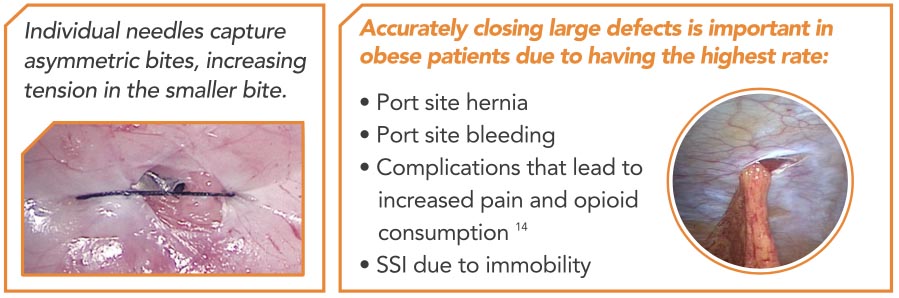
Natural movement, angled views, and the inevitable fascial tenting make symmetry difficult with individual needle punctures. M-Close is the ONLY device that simultaneously deploys two opposing needles, ensuring proper 180 degree placement every time.

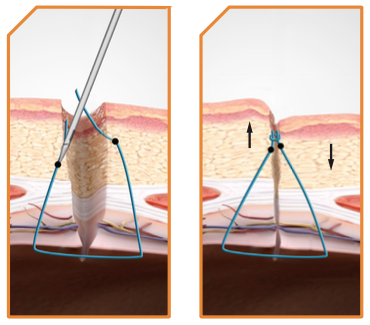
Individual Needles can cause dimpling since the needles often enter the side of the defect at different heights.
When the suture is tied the knot forces one side to be pulled toward the other creating asymmetrical tissue folds.
M-Close Kit simultaneous symmetrical needles always enter at the same height to reduce or eliminate dimpling.
Download PDF Brochure

To learn more, contact us at:
6601 Lyons Road, Suite D-8, Coconut Creek, FL 33073 T: (888)-700-8890 | F: (954)-944-2942 | info@NewWaveEndo.com
- Willschke, H et al. Ultrasonography-guided rectus sheath block in pediatric anesthesia: a new approach to an old technique. Br J Anesthesia. 2006; 97(2): 244-249
- Salinas, FV. Ultrasound-guided rectus sheath block: Clinical Anatomy. Philips tutorial. 2015
- Based on internal report: Ultrasound Analysis of the Rectus Sheath in 93 subjects. Sept. 2018
- Kim, J. Thickness of Rectus Abdominis Muscle and Abdominal Subcutaneous Fat Tissue in Adult Women: Correlation with Age, Pregnancy, Laparotomy, and Body Mass Index. Archives of Plastic Surgery 2012; 39(5)
- Crosbie, EJ et al. The surgical rectus sheath block for post-operative analgesia: a modern approach to an established technique. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2012; 160: 196–200
- Dingeman, RS et al. Ultrasonography-Guided Bilateral Rectus Sheath Block vs Local Anesthetic Infiltration After Pediatric Umbilical Hernia Repair A Prospective Randomized Clinical Trial. JAMA Surg. 2013 Aug; 148(8): 707-13
- Shah, VA et al. Ultrasound guided abdominal field blocks improve postoperative pain relief in cesarean delivery: a prospective randomized controlled study. Anesthesia Pain and Intensive Care. 2017; Vol 21(2): 218-223
- Smith, BE et al. Rectus sheath and mesosalpinx block for laparoscopic sterilization. Anesthesia. 1991; 46: 875-877
- Chazapis, M et al. Improving the Peri-operative care of Patients by instituting a 'Block Room' for Regional Anaesthesia. BMJ Quality Improvement Reports 2014
- McDermott, G et al. Should we stop doing blind transversus abdominis plane blocks? Br J Anesthesia 2012: 108 (3): 499–502
- As described in US Patent # 9,451,950 Β2
- Working Port-Site Hernias: To Close or Not to Close? Does It Matter in the Obese? Bariatric Times June 7, 2011
- Based on internal report: M-Close performance testing, July 2018
- Owens, M. A systematic review of laparoscopic port site hernias in gastrointestinal surgery. Surgeon 2011 Aug; 9(4): 218-24.
- Smith BE, Suchak M, Siggins D, Challands J. Rectus sheath block for diagnostic laparoscopy. Anaesthesia. 1988;43:947–8.